Comprehensive Nursing Care Plan for Nausea: Strategies & Management
Updated:Nausea can significantly disrupt a patient’s well-being, making the development of a nursing care plan for nausea a crucial skill for healthcare providers. This article offers a concise blueprint for nurses on assessing nausea, providing targeted care with medications, dietary adjustments, and non-pharmacological methods to relieve nausea, and continuously adapting the plan for optimal patient comfort. Embark on an instructive journey to enhance your clinical expertise to effectively manage nausea.
Key Takeaways
-
Nausea is a complex and multifaceted symptom that can significantly impact patient quality of life and requires a comprehensive nursing care plan for effective management, which includes identifying causes, assessing severity, and monitoring symptoms.
-
Effective nausea management necessitates understanding its diverse causes, ranging from gastrointestinal issues to the side effects of chemotherapy and requires rigorous assessment techniques to personalize care, including evaluating physical symptoms and gastrointestinal motility.
-
Nursing care plans for nausea should involve a combination of tailored nursing interventions, patient and caregiver education, dietary adjustments, medication management, and non-pharmacological approaches, all of which must be flexible and adaptable to changing patient conditions.
Understanding Nausea in the Clinical Setting
Nausea is more than just an unpleasant sensation; it’s a multifaceted symptom that precedes the act of vomiting and can significantly affect a patient’s quality of life. It can strike without warning and is often a side effect of various treatments for metabolic disorders and conditions, including chemotherapy-induced nausea, postoperative complications, and motion sickness. Imagine a patient undergoing cancer treatment, already burdened with the weight of their diagnosis, only to face the additional challenge of severe nausea brought on by their therapy. This is where the expertise of nursing professionals becomes invaluable.
The causes of nausea are diverse, ranging from medication side effects to psychological risk factors, each capable of triggering the vomiting reflex. It’s a symptom that doesn’t discriminate, affecting patients across the spectrum of healthcare settings—from those receiving chemotherapy to individuals recovering from surgery. Nursing diagnosis and subsequent interventions must be adept at not only treating nausea but also managing the underlying factors that exacerbate it.
Considering the debilitating nature of nausea, a comprehensive nursing care plan becomes a necessity. Such a plan not only focuses on immediate relief but also on long-term strategies to control and prevent nausea. Whether it’s through administering antiemetic medications or providing psychological support, nurses play a pivotal role in managing this symptom. This critical role underscores the importance of understanding nausea in clinical practice, as it lays the groundwork for personalized and effective patient care.
Identifying the Root Causes of Nausea
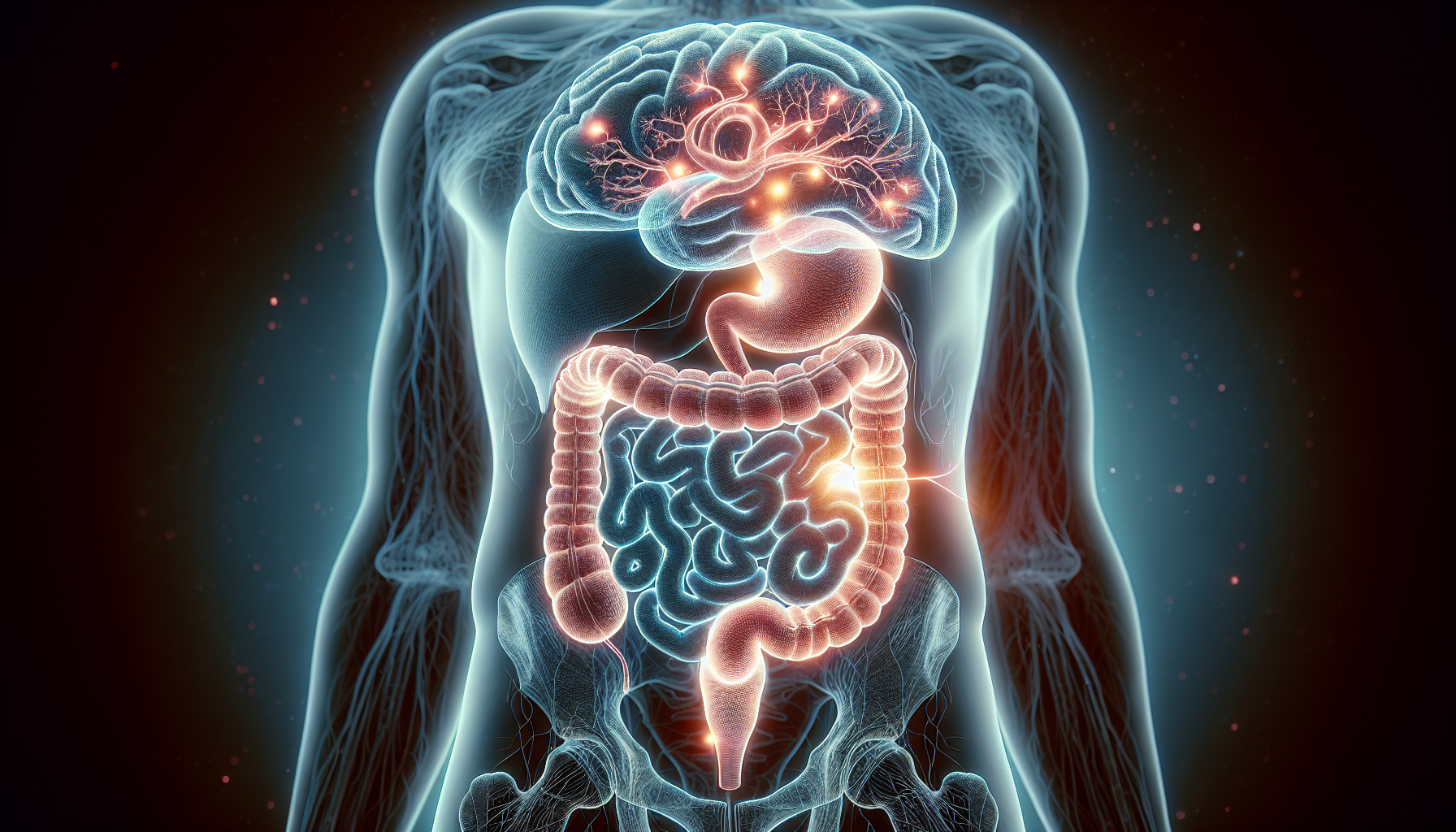
Effectively managing nausea involves understanding the complex network of potential triggers. Common causes induce nausea range from stomach flu to acid reflux, each capable of setting off a cascade of discomfort. Patients may find themselves navigating through a sea of symptoms, with nausea serving as a beacon, signaling the presence of conditions like gastrointestinal disorders, migraines, or even appendicitis. It’s a symptom that demands attention, as it could be the harbinger of a more serious underlying issue.
In the realm of gastrointestinal woes, both increased and decreased motility can play a significant role in inducing nausea prevent vomiting. The stomach and intestines, when out of sync, can trigger nausea and vomiting, serving as a distress signal that something is amiss within the digestive tract. It’s a complex interplay of factors that nursing professionals must decode to provide appropriate interventions.
The pursuit of effective nausea management is akin to a detective’s investigation—it requires piecing together clues to reveal the underlying cause. Whether it’s a straightforward case of food poisoning or a more complex condition like a bowel obstruction, understanding the root cause is the first step toward relief. With this knowledge, nursing interventions can be tailored to not only treat the symptom but also address the source, ensuring a holistic approach to care.
Comprehensive Assessment Techniques
The path to managing nausea starts with an in-depth assessment, forming the bedrock of an effective care plan. By employing tools such as visual analog scales, nurses can quantify the severity of nausea, transforming a subjective experience into measurable data. Monitoring vital signs becomes crucial in this context, as they offer a glimpse into the patient’s overall health and can indicate complications such as severe dehydration.
A comprehensive assessment goes beyond numbers, delving into the history and characteristics of nausea and vomiting. It’s about listening to the patient’s story, understanding their specific triggers, and recognizing the impact of symptoms on their daily life. This in-depth approach provides a robust foundation upon which personalized nursing interventions can be built, ensuring that each patient receives care that is tailored to their unique needs.
Monitoring Vomiting Symptoms
Vomiting accompanying nausea calls for urgent attention. The physical act of vomiting can lead to a cascade of vomiting-related issues, from fluid volume deficit to electrolyte imbalances, each with its own set of complications. Nurses are tasked with monitoring these symptoms, ensuring that patients maintain adequate hydration and receive the necessary interventions to manage any imbalances.
The characteristics of emesis—such as its content and frequency—offer valuable insights into the patient’s condition. Whether it’s the telltale signs of hyperemesis gravidarum or the increased intracranial pressure suggested by projectile vomiting, each detail helps in crafting a comprehensive and effective care plan. By closely observing and documenting these symptoms, nurses can adjust treatment strategies to ensure the patient’s comfort and recovery.
Evaluating Gastrointestinal Motility
Nausea, along with a range of other uncomfortable symptoms, can be the outcome of dysfunctional gastrointestinal motility. Nurses must evaluate these symptoms carefully, considering factors like food aversion and abdominal cramping, which are indicative of conditions such as gastroesophageal reflux disease or gastric outlet obstruction. The process of assessing gastrointestinal motility is a meticulous one, with nursing diagnoses requiring a keen eye for detail and an understanding of the intricate workings of the digestive system.
The management of gastrointestinal tract motility issues may involve interventions such as providing IV fluids or recommending dietary changes to avoid irritants. In more acute cases, where conditions like bowel obstruction are suspected, more aggressive measures may be necessary. Irrespective of the approach, nursing interventions must adapt to the patient’s changing condition, guaranteeing progress toward relief and recovery.
Crafting a Nursing Diagnosis for Nausea
A nursing diagnosis for nausea serves as more than just a label; it acts as a roadmap steering the entire care process. It’s based on the nurse’s clinical judgment and an intimate understanding of the patient’s health condition. Whether it’s the general unease of Impaired Comfort or the potential risks associated with Deficient Fluid Volume, each diagnosis is a stepping stone toward targeted interventions.
In cases where nausea impacts nutritional intake, a diagnosis of Imbalanced Nutrition might emerge, pointing to the need for strategies that address both hydration and nourishment. It’s a process that requires adaptability, as each patient’s medical history, allergies, and past experiences with treatments can significantly influence the nursing care plan.
Personalized Nursing Interventions

The mosaic of nausea management consists of personalized nursing interventions, each component depicting a distinct strategy centered around the patient’s needs. From administering antiemetic medications to utilizing positioning techniques, these interventions are crafted with precision and care.
Comprehensive Nursing Care Plan for Nausea: Strategies & Management is rated 4.8/5 based on 12 customer reviews.
Are you in need of homework help?
Place your order and get 100% original work.
Addressing patient anxieties and recommending non-pharmacological measures like ginger or peppermint tea are just as essential in the battle against nausea. By tailoring these interventions to the specific condition causing nausea, nurses ensure that each patient receives a care plan that is as unique as their experience of the symptom.
Medication Management
The administration of antiemetic medications is a delicate art, one that requires a balance between efficacy and the management of side effects. Nurses must navigate this terrain with care, monitoring the patient’s response and adjusting dosages as necessary to achieve the desired outcome.
Whether it’s in the context of chemotherapy treatment-related nausea, or managing postoperative nausea, the role of medication in symptom management is paramount. It’s a responsibility that encompasses not just the act of administering the drugs but also educating the patient on their proper use, ensuring they are equipped to manage their nausea in the most effective way possible.
Dietary Adjustments
Diet plays a pivotal role in managing nausea, and simple changes can have a profound impact on a patient’s well-being. Here are some tips for managing nausea through diet:
-
Encourage small frequent meals
-
Opt for bland, easy-to-digest foods
-
Maintain hydration
-
Ensure adequate nutrition
Following these tips can help minimize the risk of exacerbating nausea and promote overall well-being.
Collaboration with dieticians and regular assessments for malnutrition are key components of a comprehensive care plan. By taking a proactive approach to dietary management, nurses can help patients by:
-
Collaborating with dieticians
-
Conducting regular assessments for malnutrition
-
Finding a balance that supports their recovery
-
Respecting their preferences and dietary restrictions
Non-Pharmacological Approaches to Alleviate Nausea

Beyond medications, there is a world of non-pharmacological approaches that can offer solace to those experiencing nausea. Some of these methods include:
-
Ginger, which has natural healing properties and can help alleviate nausea
-
Peppermint, which can also help soothe an upset stomach
-
Aromatherapy, which uses essential oils to provide a calming influence
These methods provide a gentler way to manage symptoms.
Deep breathing exercises and relaxation techniques can serve as an anchor, steadying the storm of nausea and providing a sense of control. Similarly, acupressure and adopting an upright posture can be simple yet effective tools in the quest to control nausea. It’s a holistic approach that recognizes the power of the mind-body connection in the management of nausea.
Educating Patients and Caregivers
In the fight against nausea, knowledge is a powerful ally. Here are some strategies to help manage symptoms effectively:
-
Educate patients and caregivers on the proper use of anti-nausea medications
-
Recognize early signs of severe nausea
-
Make lifestyle changes to reduce triggers and promote overall well-being
By implementing these strategies, patients and caregivers can empower themselves to effectively treat nausea symptoms.
Open discussions and individualized education are the hallmarks of this approach, addressing practical issues and providing tailored advice to ensure patients and caregivers have the tools they need to navigate the complexities of nausea.
Preventative Measures at Home
The home environment holds a significant influence in both preventing and managing nausea. Maintaining a cool temperature, opting for bland foods, and engaging in relaxation techniques are all simple yet effective strategies that can be implemented at home.
By eliminating strong odors and creating a comfortable eating environment, patients can take proactive steps to control postoperative nausea, reduce nausea, minimize its occurrence, and enhance their overall comfort through routine oral care.
When to Seek Medical Attention
Though many instances of nausea can be handled at home, certain situations necessitate medical intervention. Persistent vomiting, severe abdominal pain, and symptoms indicative of life-threatening conditions, such as prolonged vomiting, are all red flags that warrant immediate attention.
Early intervention is key, and being aware of the signs that signal a serious underlying issue can be lifesaving. It’s a message that healthcare professionals, such as nurses, must convey to patients and caregivers, ensuring they are prepared to act swiftly when needed.
Implementing the Care Plan
The nursing care plan transcends the role of a mere document; it serves as an action plan. It organizes assessments and interventions, setting the stage for a tailored approach to managing nausea and related symptoms. The care plan must be flexible, and ready to adapt to the unpredictable nature of breakthrough nausea and vomiting episodes.
Reviewing the Treatment Plan and consulting with the Oncology team, if needed, are crucial steps in ensuring that the care plan remains aligned with the patient’s needs. It’s a dynamic process that requires continuous evaluation and adjustment, ensuring that each patient’s journey toward relief is a smooth one.
Tracking Patient Outcomes
The patient’s response is the ultimate indicator of a care plan’s success. Documenting this response is essential, as it provides the feedback needed to refine and adjust the plan. Tracking episodes of breakthrough nausea offers insights into the effectiveness of current interventions and signals when changes are necessary.
Regular updates to the care plan, guided by patient outcomes, ensure that the management of nausea evolves in step with the patient’s progress. It’s an ongoing cycle of assessment, intervention, and adaptation, all aimed at providing the highest level of care and comfort.
Summary
As we navigate the twists and turns of managing nausea, it becomes clear that this symptom demands a multifaceted approach. Every step taken is crucial in ensuring patient comfort and well-being, from understanding its roots to crafting personalized care plans. The insights provided in this guide underscore the importance of a comprehensive nursing care plan, one that is adaptable, patient-specific, and continuously evolving.
In closing, remember that while nausea is a common experience, its management is anything but ordinary. Nursing professionals' dedication to providing relief and support makes all the difference, transforming what could be an overwhelming challenge into a manageable part of the patient’s healthcare journey. May this guide serve as a beacon, illuminating the path to effective nausea management and inspiring confidence in those who walk it.
Frequently Asked Questions
What are nursing interventions for nausea?
Nursing interventions for nausea include monitoring vital signs, checking for dehydration, recommending a clear liquid diet, and consulting a healthcare provider if needed. These steps can help to manage nausea and alleviate the patient's symptoms effectively.
What are some common triggers for nausea that nurses should be aware of?
Nurses should be aware of triggers for nausea, including infections, food allergies, GERD, migraine headaches, motion sickness, excessive marijuana use, side effects from chemotherapy, and postoperative complications. These can help in identifying and addressing the cause of nausea in patients.
How can nurses measure the severity of a patient's nausea?
Nurses can measure the severity of a patient's nausea using assessment tools like visual analog scales and monitoring vital signs to assess overall health and potential complications, such as dehydration.
What non-pharmacological methods can be used to alleviate nausea?
Non-pharmacological methods such as ginger, peppermint, deep breathing exercises, and acupressure can be used to alleviate nausea. Consider trying these natural remedies to help with nausea worse relieve symptoms.
When should patients or caregivers seek medical attention for nausea?
If you experience persistent vomiting, severe abdominal pain, or symptoms of meningitis, seek immediate medical attention for nausea. These could indicate potential life-threatening conditions.
Written By
By KarenKaren hold a PhD in English (literature). She has worked as an academic tutor for more than 7 years helping students excel academically.
Place Your Order Now.
Related Posts
- ● Finance Assignment Help
- ● Accounting Assignment Help
- ● Business Assignment Help
- ● College Assignment Help
- ● Research Paper Writing Service
- ● Essay Writing Service
- ● Dissertation Writing Services
- ● Thesis Writing Service
- ● Coursework Help
- ● Statistics Assignment Help
- ● How To Write An Informative Essay
Why Choose Us
- Confidentiality and Privacy
- 100% Original Work
- 24/7 Customer Support
- Unlimited Free Revisions
- Experienced Writers
- Real-time Communication
- Affordable Prices
- Deadline Guaranteed

